White spots, butterflies and PSEUDOCATALASE. Vitiligo is a chronic skin disease characterized by depigmented (white) skin areas on the body. The disease is common and affects 1–2 percent of the population globally. Statistically, there may be many more because most people do not seek care for pigment changes in the skin.

Vitiligo vulgaris
Vitiligo vulgaris (generalized vitiligo) is the most common form of vitiligo. Vitiligo vulgaris is characterized by white patches that appear symmetrically on both sides of the body.
Segmental vitiligo
Vitiligo segmentalis is the second variant, vitiligo segmentalis (segmental vitiligo), appears as patches on only one side of the body.
Focal vitiligo
Vitiligo focalis is called the third variant and is characterized by small spots on one or a few parts of the body.
Scientists currently disagree about the reason why vitiligo occurs. Some claim that it is caused by autoimmunity, that is, when your immune system attacks the pigment cells. Others claim that a high concentration of oxidative stress destroys the pigment cells. Most likely, it is a combination of both. Patients with vitiligo (especially with vitiligo vulgaris) have antibodies against the pigment cells along with a high concentration of hydrogen peroxide, which is an oxidative marker. Which came first, the chicken or the egg? We don't know.
For a long time, it was assumed that the white spots did not contain any melanocytes (pigment cells), but now research has shown that melanocytes are still present in the white spots, they just have lost their ability to form pigment (1).
Because depigmentation can occur in visible areas of the skin, the disease can be socially stigmatizing and cause psychosocial concerns, including impaired well-being (2).

Diagnosing vitiligo is often a simple process. However, in light-skinned patients, a so-called skin lamp (Wood's lamp) may be needed to confirm that it is vitiligo. Professor Karin Schallreuter and a team of American and German researchers discovered that substances are formed in the white skin that emit fluorescence when illuminated with the lamp. These substances belong to the bioterin family and are also what give some butterflies their fluorescent color (3).

The discovery of vitiligo's ability to fluoresce was published in the prestigious journal Science in 1994 (3).
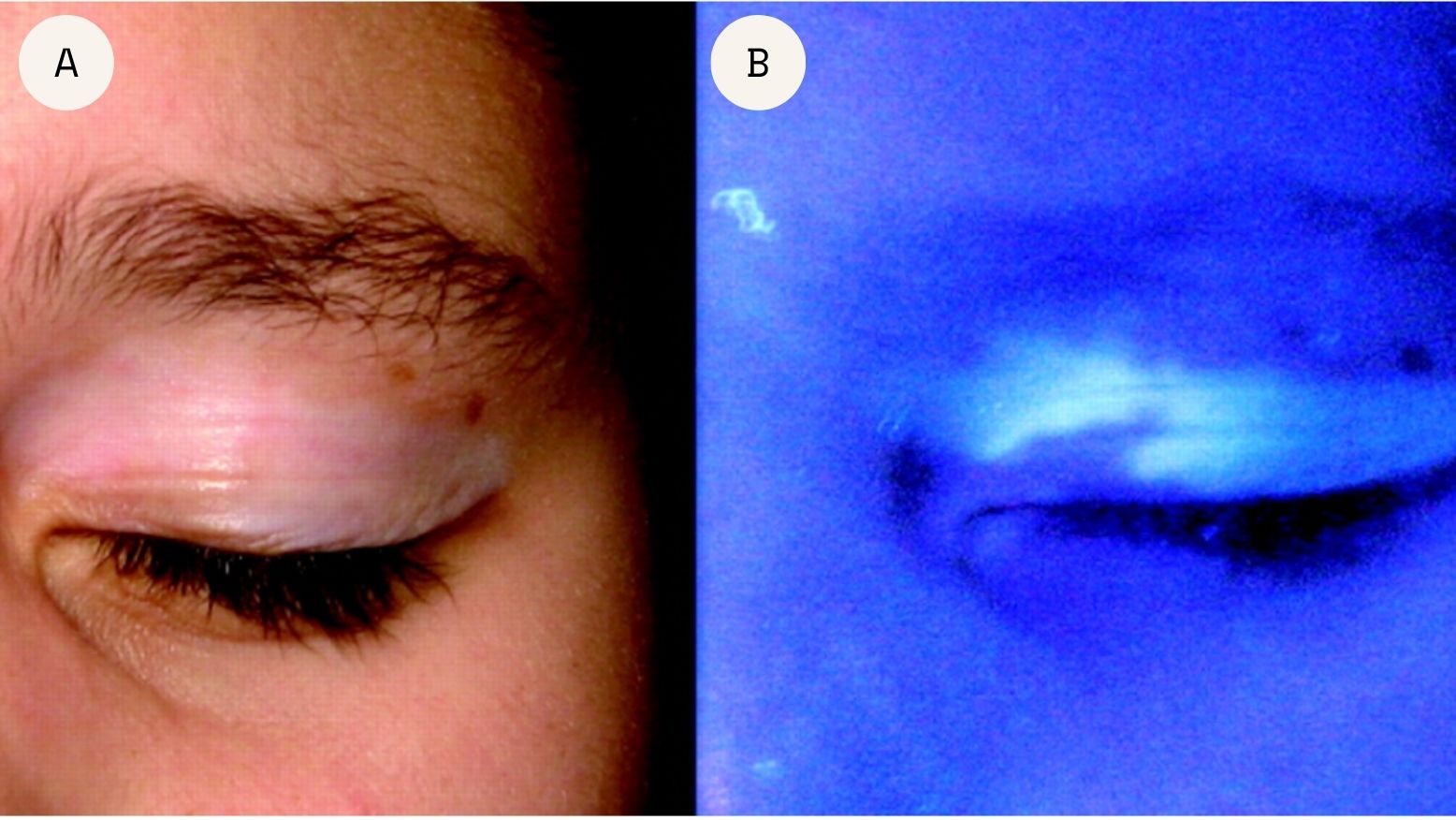
A: Vitiligo on the eyelids in visual light. B: The same eyelid under Wood's lamp produces a white fluorescent light. (4).
There are no uniform national guidelines for the treatment of vitiligo today. Most often, no further medical treatment is offered, but the focus is on patient information about the course of the disease.
However, some dermatologists prescribe cortisone or tacrolimus, a substance developed for the treatment of atopic eczema, which you are asked to apply to the affected areas. After 6 months, an evaluation is made. A few patients see some effect due to the immunomodulatory effect. A phototherapy with UVB light is recommended in some regions with varying effectiveness

This can worsen vitiligo.
Studies show that applying cream with Q10 (Inci:Ubiquinone) can worsen vitiligo (5).
This is easier said than done, but it has been shown that vitiligo is greatly exacerbated by psychological stress.
People with vitiligo are particularly vulnerable to damage and pressure on the skin, which often causes a white spot where the wound or scab used to be. This is a well-known phenomenon called the Köbner phenomenon.
Avoid tight clothing and shoes. Vitiligo often appears around the waist, under the bra, and on the feet due to constant pressure on the skin. This can trigger pigment loss.
Avoid excessive amounts of green tea as this can have pro-oxidative effects and worsen vitiligo.
Avoid smoking. Smoking has often been shown to worsen vitiligo, especially around the mouth. It is also difficult to treat vitiligo if the patient smokes because repigmentation occurs very slowly in these cases.
Professor Karin Schallreuter has studied vitiligo for the past 25 years and has been a practicing dermatologist and specialist at the Mayo Clinic, Minnesota. She is one of the founders of the Center for Skin Science at the University of Bradford and founder of the Institute for Pigmentary Disorders in Greifswald, Germany.
She has written more than 170 scientific articles in experimental and clinical dermatology and has treated more than 6,000 patients with vitiligo. In this interview, she tells us more about the treatment she has developed.
About Professor Schallreuter's treatment that has helped reduce his vitiligo.
I have had vitiligo since childhood. I visited many dermatologists and tried everything from cortisone, tacrolimus, UVB treatment to transplanting healthy pigmented skin cells into the affected areas. Nothing worked and the vitiligo actually got worse with all the treatments.
I studied pharmacy in Uppsala and graduated in 2002. During my years at university I came into contact with the German dermatologist and skin researcher Karin Schallreuter, who was a professor at the University of Bradford and an expert on vitiligo (see video clip). This contact gave me the opportunity to carry out doctoral studies in clinical and experimental dermatology with Schallreuter's team.

Based on the discovery of the “butterfly biotins” in vitiligo spots, Karin Schallreuter and her team developed a treatment to reduce oxidative stress in the skin. When the treatment was used, the melanocytes faded and started producing pigment again. Today I use NB-UVB-activated pseudocatalase PC-KUS with very good effect, my face and legs have received 90% repigmentation. However, hands and feet are still difficult to treat.
This treatment was developed by Professor Schallreuter in 1995 and has since helped thousands of patients in three different locations: Medical Clinic-The Dead Sea, Institute for Pigmentation Disorders of V. Greifswald, Germany and at the University of Bradford, England. In 2006 I defended my thesis on vitiligo and received a PhD in experimental dermatology.
Today I feel happy about my vitiligo and enjoy the white patches, even though several of them have now completely disappeared. If I hadn't had them, I probably wouldn't have had the motivation I have, nor would I have experienced all that I have experienced or met all these amazing people and researchers that I have met over the years.
If you are interested, please read the scientific publications about the treatment here .
/Johanna Gillbro




